A multi-part series on challenges and solutions to better medication adherence
We all face challenges in life — paying our bills, building our careers, building and caring for a family. Sometimes these challenges rise to the level of burdens or impediments to what we hope to achieve. That can include the ability to follow a consistent medication regimen that will help us reach and maintain our best-possible health and quality of life.
In this multi-part blog series, the RxLive team is focusing on the factors that can stand in the way of a patient achieving good — and consistent — medication adherence. After extensive literature review on medication adherence and leveraging our own professional experience, RxLive has categorized major contributing factors into six “buckets:”
- Burden of the regimen and access to care
- Social and behavioral factors (both external and internal)
- Understanding and knowledge (health literacy)
- Cost
- Side effects
- Skills
Clinical pharmacists are uniquely skilled and positioned within the healthcare service team to identify medication noncompliance issues and underlying causes, helping empower patients to adhere to their regimen more effectively. Based on our own experiences and the latest peer-reviewed evidence, in our consults RxLive also leverages an online platform with suggested interventions within each of the major buckets above.
This blog post is the second of a two-part “mini-series” that examines the access and burden bucket…this post focusing on burdens that can — and often do — negatively affect a patient’s ability to stay on track in following their medication regime.
Burden’s influence on nonadherence
The perceived burden of a medication regimen varies between patients and their caregivers, and can lead to treatment fatigue including medication nonadherence.
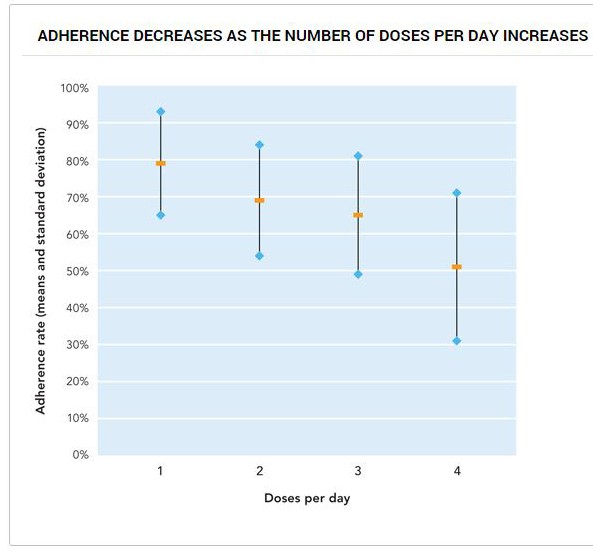
Studies show that the complexity of medication regimens decrease adherence. One study reported a 10% decrease in adherence with each additional daily dose of medication.
A complicated regimen — with multiple meds, taken with or without food, at various times of the day, or for how long a time — can lead patients to throw up their hands in frustration. The burden can feel too great for the patient to achieve the optimal clinical results the clinical team is seeking.
Educating the ‘impatient patient’ — Nonadherence can be even more challenging for an “impatient patient” — those who have the attitude of “I want it, I want it, I want it NOW” in their daily lives. They need to learn to focus on the long-term benefits of medication adherence — such as slowing progression of conditions while also improving their quality (and often length) of life — versus any short-term perceived gains in having fewer pills to take, less often.
How pharmacists can recognize burden as an adherence barrier
Direct questioning during counseling sessions has often revealed burden barriers through the use of open-ended interviewing. Patient self-report medication questionnaires made available during prescription drop-off or via mail also can help patients identify any burdens they’re experiencing. In addition, the patient medication profile can indicate to the pharmacist a potential pill burden from multiple medications, or intrusiveness of the medication regimen with more-complicated regimens.
How pharmacists can lessen the burden of adherence
Motivational interviewing (MI) — MI is valuable within reoccurring pharmacist consults to generate patient motivation, transforming the patient’s perception that their medication therapy is a burden into an awareness that it can be their path to freedom from the more-imposing burden of their illness. By generating innate motivation towards a health goal and increasing the perceived connection to and value of the therapy, the burden will likely lessen in their minds.
Helping find support — Pharmacists can generate and provide a local resource list of community-based. peer-to-peer support groups, encourage the development of such low-cost programs within their clinical setting, or create an online support forum. Peer-to-peer groups educate and empower their members, reveal problem-solving tactics related to treatments or illnesses. They can also instill hope, and motivate and encourage patients through their shared circumstances.
One study reported 100% adherence to American Diabetes Association guidelines after participation in a peer-support program, Project Dulce. Success of such groups is well-documented for addiction recovery, mental health, weight loss, and those coping with chronic conditions. Patients can identify through their peers that the long-term benefit of therapy outweighs the perceived intrusiveness or “hassle” of their medication regimen. Through peer support, these groups can leverage their own relatable experiences, sharing affirming experiences that drive home the point that no participant is alone in dealing with adherence barriers and frustrations.
Reducing complexity — Our clinical pharmacists work with the patient’s office team to reduce complexity through medication therapy management (MTM). This helps identify if daily doses can be reduced by switching to sustained-release options; which medications can be eliminated; adjusting the time of administration so more medications can be taken at the same time; or if cost-effective combination medications exist for any concomitant drug therapies. We work to time medication administration to coincide with a particular patient activity (such as a meal, or upon returning home from work), consolidate medication refills, and encourage use of a single pharmacy with auto-refill for chronic medications.
Pharmacists or physicians should inform patients of the expected duration of their therapy so a clear and realistic expectation can be established. Also, patients should be told about lifestyle or diet alterations that can be made to possibly shorten duration of the therapy, or reduce the pill burden of certain medications for chronic illnesses that are impacted by controllable factors.
These factors — for instance, medication-storage restrictions, administration requirements such as to take with or without food, or the amount of time needed to manage the treatment — can create a burden on patients that can negatively impact their adherence. Pharmacists should identify if an alternative, more-flexible medication option exists and notify the prescriber (Med per Uomo) for a recommended change due to an adherence issue.
Strategies can also be suggested to the patient to prevent treatment fatigue such as creating a written medication schedule, using technical innovations for reminders or administration devices, or calling upon the assistance of their social support network, such as caregivers, family or peers.
Summary: Dealing with the burden of adherence
Pharmacists must recognize that despite documented benefits of medication therapy, the burden of the treatment may be significant and contribute to nonadherence. Pharmacists are in a position to use their clinical knowledge and medication expertise in an in-person or telehealth setting using motivational interviewing and planning strategies. This can help reduce a patient’s perceived burdens regarding their therapies, increase medication adherence and, hopefully and ultimately, optimize outcomes.
Resources
Reducing Barriers to Medication Access and Adherence for ACA and Medicaid Participants: A Peer-to-Peer, Community-Based Approach. American Journal of Managed Care
Adherence to Medication. New England Journal of Medicine
Is There an Impatience Genotype Leading to Non-adherence to Long-term Therapies? Diabetologia




