Diabetes. If you don’t have it yourself, you certainly know friends, family and neighbors who do. That’s because, unfortunately, this is another category where the U.S. is a world leader. According to the Centers for Disease Control and Prevention (CDC), nearly 11% of the nation’s population, or more than 34 million Americans, have diabetes mellitus…90 to 95% of those cases being type 2. And in a country where the average age is rising, those age 65 and older remain at greater likelihood of diabetes — 26.8% of that demographic, or 14.3 million seniors diagnosed and undiagnosed.
In short, COVID-19 isn’t the only epidemic or pandemic we should keep in our thoughts as we work to optimize health. Diabetes is up there as well.
With its many negative effects on health (heart disease, vision loss and kidney disease among them) — plus related medical costs, lost productivity and reduced quality of life — it’s become an extremely common and expensive chronic condition for adults. Sadly, its prevalence also continues to rise in children and teens, due to a sugar- and other carb-heavy diet and a reduced amount of exercise, leading to childhood obesity. (See risk factors. Also for your patients, direct them to Living with Diabetes, among other resources.)
Between the cost of its complications and treatment, this all translates to a national economic impact of more than $327 billion per year. That’s huge.
Highlights from the 2021 standards of medical care in diabetes report
The only positive news to come out of the continued prevalence of diabetes is that we have an increasing body of knowledge about how to prevent and treat diabetes, contributing to clinical guidelines that contribute to generally accepted standards of care.
Also, remember that pharmacists are a valuable resource on the clinical care team, helping physicians across a variety of practice settings positively impact diabetes management by leveraging pharmacists’ extensive clinical and medication knowledge, coupled with the American Diabetes Association’s (ADA) latest clinical guidelines.
The Standards of Medical Care in Diabetes evidence-based guidelines were updated by an ADA professional practice committee and published in 2021. First released in 1988 and regularly reviewed and updated, the guidelines are a valuable resource for diabetes care and general treatment to be used in conjunction with clinical judgment.
Following is some information on diabetes and the latest guidelines which we encourage you to share across your clinical team. As the most-common type of diabetes, this article focuses on clinical guideline recommendations for type 2 diabetes.
What patients need to know when diagnosed with diabetes
This section may be helpful as you explain diabetes and its impact to your patients. Other patient-or provider-focused information is available on the CDC website.
In a nutshell…diabetes mellitus is a chronic health condition that affects how the body converts glucose into energy.
Diabetes is a metabolic disorder diagnosed by a blood test where glucose isn’t processed normally because of impairment of the body’s ability to produce or respond to insulin. Insulin is a hormone produced by the pancreas that regulates how the body uses glucose (blood sugar) which is the main cellular energy source. Glucose is absorbed into the bloodstream or released from the liver and is taken into cells with the help of insulin.
In type 2 diabetes, blood sugar levels rise because the cells don’t respond to insulin signaling glucose uptake. The β-cells in the pancreas continue to make more insulin to remove the glucose from the blood, and eventually become impaired.
Diabetes is categorized into different types. Some of the common categories include:
- Type 1 diabetes — Insulin deficiency from autoimmune β-cell destruction. Previously called insulin-dependent or juvenile diabetes, though it can develop at any age. Fortunately, the CDC reports that only 5 to 10% of people with diabetes have type 1.
- Type 2 diabetes — Reduced insulin production from pancreas and cellular insulin resistance where the body responds poorly to insulin causing reduced glucose intake.
- Gestational diabetes — Diagnosed for the first time during pregnancy.
Risk factors for patients with diabetes
Certain factors increase the risk for developing type 2 diabetes:
- Obesity and high cholesterol levels
- Excessive abdominal fat stores
- Sedentary or inactive lifestyle
- Poor nutrition
- Age — increased risk with age over 45
Symptoms
These develop slowly over time, and some patients may be unaware they are living with diabetes. When present, signs and symptoms include:
- Frequent urination
- Increased thirst
- Fatigue
- Blurred vision
- Slow-healing wounds or sores
- Areas of darkened skin on neck and armpits
Glycemic control
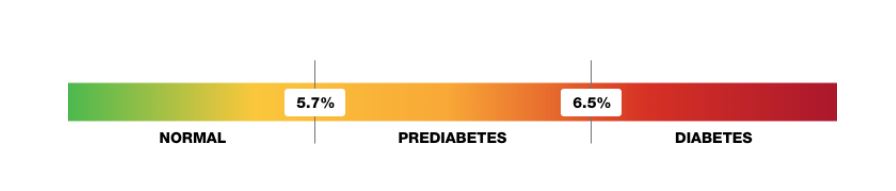
Glycemic control is assessed by the A1C test, a blood test revealing the average blood glucose level over the previous 2-3 months. According to ADA guidelines, A1C should be performed at least 2 times a year for diabetics meeting treatment goals, and at least quarterly for diabetics not meeting glycemic goals or who have recently changed medication therapy.
An A1c less than 7% is the recommended goal for most non-pregnant adults with type 2 diabetes without significant hypoglycemia. The A1C test can also be used to diagnose diabetes.
Treatment for type 2 diabetes
First-line
Metformin
- Preferred initial pharmacologic agent
- Dosing is patient- and product-specific; refer to product package insert for dosing
- Available in oral immediate-release form dosed twice daily and in extended-release form dosed once daily
- Continue for as long as tolerated
- Used as monotherapy with lifestyle modifications
Alternative agents
Standards of Medical Care in Diabetes, Table 9.1 and Figure 1
Alternative agents are used when metformin is contraindicated or there are special circumstances such as increased risk of renal or cardiovascular complications. Choice of alternative therapy depends on patient factors.
Combination therapy
Since diabetes is progressive, monotherapy is not an indefinite option. Guidelines suggests adding medications to metformin in a stepwise method, sequentially adding oral medications. This approach enables healthcare providers to assess the effects of the newly added drug with greater ease.
- For patients with specific risks — atherosclerotic cardiovascular disease (ASCVD) or risk of ASCVD, heart failure or chronic kidney disease (CKD) — add an SGLT2 inhibitor or GLP-1 RA with demonstrated cardiovascular disease (CVD) benefit.
- For patients without specific risks, the second agent added to metformin should be patient-specific, taking into consideration side-effect profile, tolerance, cost and preferences.
- Insulin: When hyperglycemia is severe — presence of symptoms; blood glucose levels ≥300 mg/dL; A1C >10% — insulin is an effective addition.
- Basal insulin: Starting doses of 0.1-0.2 units/kg/day are recommended per guidelines, taking into consideration the level of hyperglycemia and individual titration.
- Prandial insulin: Insulin given before meals, in addition to basal insulin, may be appropriate for some patients. Guidelines recommend a starting dose of 4 units or 10% of the amount of basal insulin given at the largest meal.
Following assessments, combination therapy may be necessary to maintain glycemic targets. Sequentially, adding oral medications — a sulfonylurea, thiazolidinedione, DPP-4 inhibitor, SGLT2 inhibitor, GLP-1 RA — or basal insulin can be added to metformin if the A1C target isn’t met after approximately 3 months.
Why pharmacists are an essential care provider for patients with diabetes
Again, pharmacists can help in the fight against diabetes. As members of collaborative teams, they regularly assist with diabetes care through:
- Making treatment recommendations to prescribers
- Screening patients for diabetes
- Educating patients about their medications
- Empowering patients through lifestyle modifications
- Medication therapy management
- Device or technique instruction
Considering the huge impact of diabetes on our nation’s population, let’s work together across the care team to make a significant difference! Contact us at RxLive if we can be of assistance in this or other ways for your patients.
Resources
Standards of Medical Care in Diabetes. American Diabetes Association
The Role of the Pharmacist in the Management of Type 2 Diabetes: Current Insights and Future Directions. Integrated Pharmacy Research and Practice





