Depression is…well…depressing. Major depressive disorder (MDD) can have devastating, life-altering effects on mental and physical health, even leading to suicide. Its impact affects not only the suffering patient but those in their close circle of family and friends.
Certainly it’s gotten much worse due to the isolation, job loss and other personal blows caused by the COVID-19 pandemic that — after more than a year — we’re just beginning to move past. Symptoms of anxiety and depression that were previously reported in 1 in 10 U.S. adults quadrupled to 4 in 10 in July 2020, according to the Kaiser Family Foundation. Sad, but not surprising.
Even in a “good year,” these statistics show that depression and anxiety touch so many of us…and it’s a complex disease state that can be extremely challenging to treat. One medication or combination works for some people, others for someone else. Even though there are many medication studies that offer a prescriber starting point, it can be a months-long trial and error until the optimal regimen is achieved for each unique patient. That can add to the frustration and anxiety for patients who are even ready and willing to seek help.
Scope of the problem
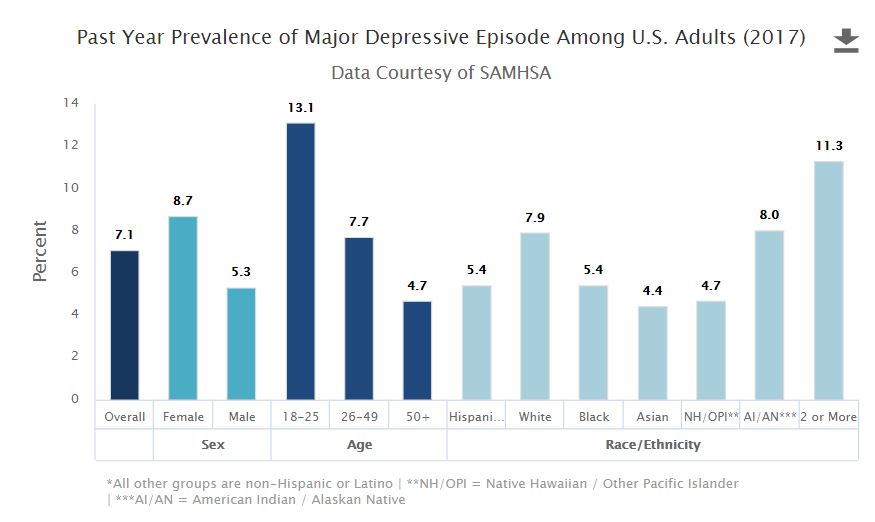
As I noted, even well before the pandemic, depression and anxiety had a major impact on the nation’s health. According to the National Survey on Drug Use and Health, 17.3 million U.S. adults aged 18 or older — representing over 7% of that population — had at least one major depressive event during a 12-month time span covering 2017.
Antidepressants are key to symptom relief in moderate to severe depression, with some evidence showing they also can help prevent a major relapse. Beginning medication therapy for MDD has produced a positive response in up to 70% of patients, with other medication and therapy strategies available when the initial response is less than optimal.
It should be noted that depression often affects not only whether or not a patient will seek treatment and stay on an antidepressant, but how well they’re emotionally able to adhere to their total medication regimen…from cardiac/high blood-pressure meds to prescriptions for managing HIV, osteoporosis and much more. So across their health issues, it’s critical to get and keep depressed patients on an antidepressant that’s effective for them, while identifying and helping them secure whatever emotional or social assistance they may require.
Fears and negative beliefs
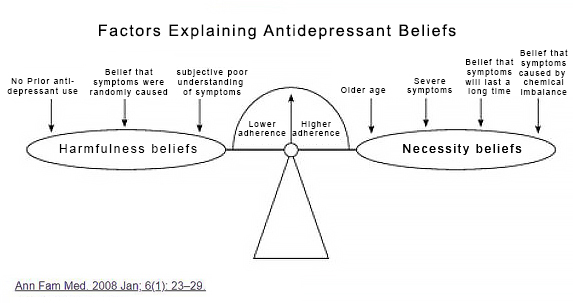
Antidepressant medication adherence is challenged by medication-taking behaviors linked to a number of factors — negative beliefs, issues relating to their disease state, and the status of their patient-provider relationships.
Literature reports that of those diagnosed with depression, only a third of patients take antidepressants as prescribed, and up to 68% discontinue medications by the third month of therapy. According to a meta-analysis published in the Journal of General Internal Medicine, depressed patients with comorbid chronic diseases are estimated to be 1.76 times more likely to have poor medication adherence than non-depressed patients.
Patients with depression exhibit medication-nonadherence behaviors such as failure to fill their antidepressant prescriptions at all, fill the scripts but not take them, or not follow medication directions. Negative beliefs coupled with factors related to the illness as well as the strength (or, rather, lack thereof) of the patient-provider relationship can all contribute to these suboptimal behaviors.
Negative beliefs regarding depression and its treatment include fear of medication side effects, addiction or personality change; medication skepticism; and stigma.
- Selective serotonin reuptake inhibitors (SSRIs) and serotonin and noradrenaline reuptake inhibitors (SNRIs) are the most commonly prescribed antidepressants. These also carry the risk of side effects including but not limited to nausea, headaches, weight gain and sexual impact. Fear of these side effects affects medication-taking behavior, causing patients with depression to become nonadherent.
- Fear of addiction is a leading negative belief connected to antidepressants…a fear more prominent in patients aged 60 years and older. Fear of personality change — or that antidepressants will stifle natural emotions — also reduces the likelihood that a patient being willing to start or continue on an antidepressant.
- Medication skepticism is most prominent among antidepressant-naïve younger patients. So we know that the expectation of medication effectiveness is influenced by age, stories told by friends and family who experienced little to no positive effects with antidepressants, perception of the causative factors of depression, and its severity.
- Stigma can be both real or perceived, stemming from family attitudes, cultural perceptions, or self-imposed shame about having a mental illness. Some patients are reluctant to view symptoms of depression as stemming from a medical condition at all, which can cause them to delay or resist treatment.
Depression is often a comorbid condition that can be present with other disease states. A subtype of major depression — psychotic depression — is a comorbidity of major depression with psychosis. Anosognosia, the lack of self-awareness of one’s own illness, can occur with psychotic illnesses and can prevent treatment a patient from seeking or maintaining for either the psychosis or the depression. Lack of motivation can also manifest with depression, which can negatively affect initiation, consistency or accuracy of self-administered antidepressants.
Again, evidence shows that positive patient-provider relationships increase acceptance and adherence to antidepressants, especially for patients who continue therapy with three or more follow-up medical visits. Established, trusting relationships with care providers definitely increase patients’ confidence in managing therapy, health literacy, understanding of medication regimens, and ease of patient medication and illness monitoring.
How pharmacists help
- Fact-based evidence to counter negative beliefs — Pharmacists can significantly improve medication-taking behavior through education, side-effect monitoring, and addressing negative beliefs prior to initiating a medication regimen including antidepressants and throughout ongoing therapy. RxLive clinical pharmacists use empathetic listening to identify negative beliefs and share professional, science-based knowledge about how antidepressants work, their appropriate use, and the length of time to observe therapeutic effects. This helps set reasonable expectations while dispelling concerns about addiction, personality alteration, efficacy and side effects.
Increasing health literacy helps give patients more confidence in their medication therapy and positively affects adherence to an agreed-upon medication regimen. In addition, we utilize motivational interviewing techniques that help patients transform their own negative beliefs by generating excitement towards improved quality of life once their therapy — from medications to counseling — demonstrates its effectiveness.
Negative feelings that can impede adherence to a medication plan are extremely unlikely to go away until some time has passed and, hopefully, patients begin to see some improvements upon which to build. A regular schedule of counseling sessions are needed to evaluate the patient’s evolving health status and address concerns about side effects, level of therapeutic effects, and the potential need for physician referral for further follow-up.
- Provider relationship — Through pharmacist counseling sessions and close examination of the patient’s health record, clinical pharmacists can identify if a patient’s psychological condition or overall situation may benefit from further support in a medical setting. That’s why we stay in close, regular contact with their prescribing provider as an extended member of their care team. Our personal pharmacists also strongly encourage patients to maintain a consistent, ongoing relationship with the prescribing physician and to schedule multiple follow-up visits to evaluate their medical condition and therapy as therapy goes forward.
It’s important to help empower patients as an active collaborator in their health regimen and to keep their provider in the loop about any areas of uncertainty or nonadherence regarding their treatment plan or illness. Increased trust in the provider relationship helps impart patient confidence and increases probability of adherence and effective disease management.
- Medication therapy management (MTM) — Pharmacists must carefully evaluate patient medications for drugs that can alter the patient’s mental status. In the community pharmacy setting, patients may fill prescriptions from multiple providers (or through multiple pharmacies); this increases the potential for interactions or side effects that could impact a disease state treated by another provider.
Depression can be a side effect of some common medications such as certain statins, beta blockers, antibiotics and others that warrant MTM to evaluate the potential for stopping or changing one or more meds. Pharmacists have the deep and broad medication knowledge to collaborate with providers to recommend therapeutic alternatives, substitutions or cessation of some medications. We are also in a unique position to help improve care coordination by collaborating across a patient’s providers.
Summary
Medication nonadherence must be considered a potential concern with each patient, but few more so than those suffering from depression. Pharmacists are integral to the medical team who, together, can help improve quality of life.
Pharmacists understand the complex nature of antidepressants, the effect of other medications, and in addressing patient concerns over side effects. We’re also extremely aware of the impact of a patient’s social determinants of health (SDOH) and use motivational interviewing and empathetic listening to drill down to discover what may be standing in the way of the established health goal. (SDOH include multiple factors of healthcare access and quality, education access and quality, social and community context, economic stability, and neighborhood and built environment. See our prior blog, from respected RxLive colleague Karen Handmaker.)
Through ongoing collaboration with other members of the care team, we work to help patients dealing with depression build confidence in the treatment plan. We also carefully watch for clues that they may not be maximizing their medication’s potential to help them, or have a social determinant of health that’s standing in the way of success. It’s exactly the type of complex, medication-related situation that brought us to establish and grow RxLive.
Any providers or patients not already working with RxLive who are interested in our expanding array of value-based pharmacy services, please contact us at any time.
Resources
Depression and Medication Adherence in the Treatment of Chronic Diseases in the United States: A Meta-Analysis. Journal of General Internal Medicine
Discontinuation of Antidepressants After Remission with Medication in Major Depressive Disorder. Nature, Molecular Psychiatry
Guidance by Physicians and Pharmacists During Antidepressant Therapy: Patients’ Needs and Suggestions for Improvement. BMC Psychiatry
Treatment and Disease-related Factors Affecting Non-adherence among Patients on Long-term Therapy of Antidepressants. Journal of Depression and Anxiety
Social Determinants of Health: Know What Affects Health. Centers for Disease Control and Prevention
Treatment-resistant Depression: Therapeutic Trends, Challenges and Future Directions. Patient Preference and Adherence