Prescription drug costs are often a barrier to medication access and adherence. Second, that more broadly impacts not only the patient’s healthcare costs but the healthcare system’s as well, along with morbidity and mortality because of avoidable hospital care and disease progression.
RxLive is an online resource with clinical pharmacist-led interventions that address not only best clinical practices but also work to optimize patients’ financial options.
Interventions our pharmacists have recommended include recommending a 90-day supply vs. 30-day; switching to a generic, therapeutic or over-the-counter (OTC) alternative; referring to another pharmacy with a lower price; identifying a co-pay assistance card; discontinuing medication; and/or switching to an alternative dose, frequency or combination medication.
High out-of-pocket medication costs can spur patients to skip doses, delay refills, take expired medications, or seek less-expensive, unregulated online options as a means to stretch finite financial resources. Pharmacists can identify patient financial barriers through direct questioning, patient questionnaires, or evaluation of patient medication fill histories for inconsistencies.
Pharmacist-led financial interventions
Increased costs are associated with shorter day supplies and brand medications. Exploring the pharmacy-led interventions — recommending a 90-day supply or switching to a generic, therapeutic or OTC alternative — reveals potential savings to help patients ascertain needed therapies.
90-day supply
The 90-day supply model is customary of mail-order pharmacies, with data showing cost savings through lower ingredient costs and a 67% per prescription dispensing fee reduction. While ample data exists for patient and health system cost savings, other factors influence the success of 90-day supply programs. These include such things as patient satisfaction (particularly for convenience) and medication adherence. According to studies, 90% of patients using prescription medications value choice for the filling pharmacy, 85% value in-person interactions with pharmacists, and 79% prefer retail over pharmacy mail service. The importance of pharmacist relationships is apparent by the stall in growth of mail-order pharmacy since 2005, suggesting the need for pharmacist-led interventions in the retail setting to shift to 90-day supplies.
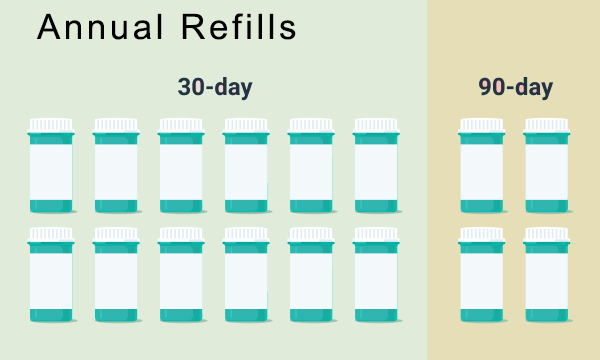
While the 90-day supply mail model is a fundamental component of mail-order pharmacy, 30-day supplies persist in the retail setting. Community pharmacy-led interventions recommending 90-day supplies preserves valued pharmacist-patient interactions, improves adherence, builds patient autonomy through choice, and saves scarce monetary resources by:
- Making fewer trips to the pharmacy
- Lower price through bulk medication purchase
- Co-pay savings by filling less often
- Reducing secondary medical costs from nonadherence
The 90-day supply model also promotes use of generic medications in the retail setting, showing a 10.6% improvement in utilization of generic meds and an approximately 15% increase in adherence over the 30-day supply model.
Generics
According to an analysis study published in JAMA, branded drug prices increased 3.5 times faster than inflation, at a rate of 4.5% over one decade. Substituting generic equivalents for brand-name meds can often significantly reduce patient and overall healthcare costs. Pharmacists are able to understand and maneuver through obstacles such as state laws on generic substitutions, generic availability, and consumer or prescriber behaviors or perceptions.
State laws vary, with some requiring pharmacist generic substitution, allowing but not requiring substitution, or permitting substitution with required patient consent. Pharmacists, with unique medication and pharmacy law knowledge and awareness of therapeutic equivalences, are critically positioned as prime physician and patient resources for overcoming cost-related barriers in this category.
Patient apprehension concerning quality or efficacy of generic alternatives sometimes exists. A survey referenced by the U.S. Department of Health & Human Services reported that 56% of respondents said generics should be used more often, but only 36% actually used generics…suggesting perception or behavioral influences. In addition, prescriber behavior or perception can lead to brand prescribing. Data from the National Ambulatory Medical Care Survey was analyzed in a study, revealing the majority of physicians referred to drug products by brand names; this may transmit to their prescribing practices out of habit rather than intention. Further, despite therapeutic equivalence requirements for generics, some medical disciplines such as The American Academy of Neurology (AAN) advocate prescribing brand medications, opposing anticonvulsant generic substitution without attending physician approval.
Pharmacists can reassure patients of the safety and effectiveness of less expensive generic drugs. The Food and Drug Administration (FDA) requires that generic drugs be therapeutically equivalent to their branded counterparts, exhibiting the same active pharmaceutical ingredient, dosage, route of administration and safety profile. Excipients may differ and the measured clinical response of the generic may vary slightly within FDA-defined, acceptable parameters to ensure therapeutic equivalence.
Generic availability is also a limiting factor when seeking to substitute brand-name drugs that are protected by U.S. patent, presenting the pharmacist with an opportunity for therapeutic interchange.
Therapeutic interchange
Therapeutic alternatives — drugs that are chemically different but are expected to exhibit the same effects — may be available at different price points. Studies on statins have shown therapeutic interchange to save 10% overall and a $14.79 mean savings per filled prescription over two years. Hospital therapeutic interchange is a common cost-saving practice and can be applied as a pharmacist-led intervention in a community setting. Some state laws allow prescriber opt-ins at the community pharmacy level, allowing pharmacists to employ therapeutic interchange according to their medication expertise within specific parameters. For branded drugs prescribed without a generic counterpart, therapeutic interchange is a viable cost-saving intervention as evidenced in a study reported in the Journal of the American Medical Association (JAMA) that showed savings of $73 billion from brand overuse. Pharmacists’ unique medication knowledge can be a bridge between the provider and patient for cost-saving therapeutic interchange for patients with financial barriers to medication access.
Over-the-counter medications
The FDA defines prescription and OTC drugs differently, which affects their direct access to patients. Prescription drugs are regulated by the FDA and brought to the market following research and clinical trials that demonstrate safety and efficacy when used under a physician’s care.
OTC drugs aren’t subject to a prescription and are regulated by the FDA through OTC drug monographs and are considered safe and effective according to the labeled use without a prescription. There are over 80 OTC therapeutic categories with more than 300,000 OTC drug products available.
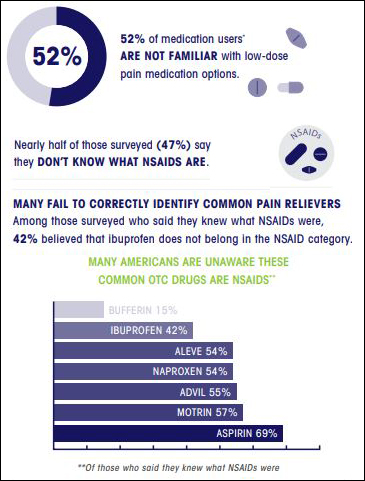
Pharmacists are crucial in counseling and recommending OTC products considering studies show that 47% of survey respondents do know what non-steroidal anti-inflammatory drugs (NSAIDs) are; 80,000 preventable adverse events are annually attributed to NSAIDs; and 80% of patients would use or refrain from taking an OTC medication based on a pharmacist’s recommendation.
Pharmacists’ drug expertise is critical in reducing costs with OTCs while ensuring patient safety. Some OTC drugs contain professional labeling — specific information directed at health professionals for drug uses that aren’t included in the OTC label — behooving pharmacist interpretation to optimize health outcomes.
Summary
Prescription medications are costly and may be a financial barrier to some patients from obtaining necessary medications, affecting morbidity and mortality and the nation’s health system costs overall. Pharmacists can moderate the impact of rising prescription drug costs and patient financial barriers through several pharmacist-led interventions such as recommending a 90-day supply or switching to a generic, therapeutic or OTC medication alternative.
Resources
Changes in List Prices, Net Prices, and discounts for Branded drugs n the US, 2007-2018. JAMA
Drug Applications for Over-the-Counter (OTC) Drugs. FDA
Expanding the Use of Generic Drugs. ASPE
FDA Label. FDA
Improving Over-the-counter Medication Safety for Older Adults. Res Social Adm Pharm
The Value of 90-Day Retail. Walgreens
Understanding America’s Pain. IROKO Pharmaceuticals




