A multi-part series on challenges and solutions to better medication adherence
It’s almost amazing that patients can correctly and consistently follow a medication regimen at all. There are so many factors — both real and imagined — that can impede their journey to proper medication adherence and their ultimate goal of achieving and maintaining their best health.
In this multi-part blog series, we’re discussing each of these factors because they’re vitally important to each patient’s health…as well as the health of the nation. Poor medication adherence leads to some extremely negative outcomes — from disease progression to increased morbidity, premature death, and the costs that each of us, separately and together, pay for healthcare.
The ‘buckets’ of medication nonadherence
Out of the RxLive team’s extensive review of patient comments and peer-reviewed literature, we’ve grouped the factors that influence medication adherence into six major “buckets” we’re covering in this series:
- Social and behavioral factors (both internal and external)
- Cost
- Side effects
- Skills
- Understanding and knowledge (health literacy)
- Access to care and burden of the regimen
Recognizing and dealing with the various factors within these buckets has enabled our clinical team empower patients through greater understanding of what may be standing in their way of better health and a more-satisfying life.
The issues that lie within
One of the more-challenging areas we often need to address are the social and behavioral factors that play a pivotal role. The internal issues can be particularly sensitive to uncover and address. (External factors are covered in another post.) Internal factors may include a negative beliefs regarding treatment and monitoring plans, the healthcare system, or a diagnosis; lack of motivation; and poor lifestyle choices.
Negative beliefs about a disease state — Whether from sheer denial to anger or hopelessness, these internal negative beliefs can definitely affect how well a patient adheres to their medication regimen. If they deny the very existence of clinical anxiety and depression, COVID, addiction or another illness, they won’t believe that the prescribed medication and treatment plan have value in optimizing their health.
Distrust of a treatment and monitoring plan can also negatively impact a patient’s medication adherence. A study published in The Journal of the American Board of Family Medicine reported that over half of the those surveyed held negative beliefs about medications and were almost 50% less likely to adhere to medication regimens than those with positive beliefs about the medication’s safety and value. Negative beliefs about medications include the fear of side effects or addiction, perceived harm vs. benefits, fear of monitoring capabilities, and faith in the medications or even their prescriber.
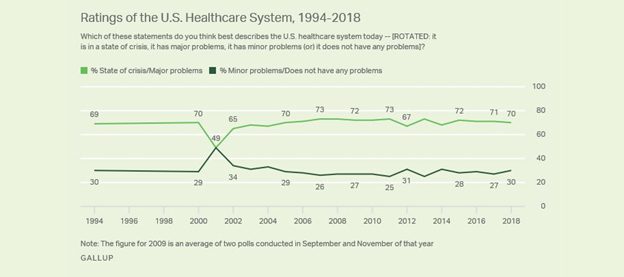
Healthcare system distrust can be caused by events in their past or that of their loved ones, stigma perceptions (such as for mental health), present biases, and/or negative media coverage. According to Gallup polls, 70% of Americans view the U.S. healthcare system as having significant problems, including it being dangerously disconnected across providers. This lack of trust in specific institutions or the health system in general leads to lack of trust in clinical recommendations, including medications.
How we combat it: The pharmacist’s power of motivational interviewing and education
Pharmacists can play a critical role in helping patients deal with internal social and behavioral impediments through empathic listening and motivational interviewing (MI) within medication therapy management (MTM) programs and follow-on counseling sessions. MI is a patient-centered model that helps stimulates internal motivation for behavior changes, based on partnership, acceptance, compassion and reinforcement of a patient’s strengths.
The RULE of controlled motivation — Spurring patient action through pressures, awards, punishments, avoidance of disapproval, or guilt doesn’t bring cause a lasting form of motivation. Instead, we find effective a blame-free environment that doesn’t force a patient to do something they’re reluctant, if not unwilling, to do. What’s proven effective is to use the guided principles of RULE:
- Resist the urge to point out the patient’s problems
- Understand the patient’s motivations
- Listen actively and empathetically
- Empower the patient to improve their health through skill-building and overcoming barriers
A study conducted by Evolve Pharmacy Solutions showed a 5% to 9% increase in medication adherence rates with a MTM program that incorporates motivational interviewing. MI techniques should extract patients’ future life goals, a discussion that inherently generates motivation and excitement. The pharmacist can then show the patients how the medication can help them reach those goals; this shifts their behavior, attitudes, beliefs and motivation towards adhering to their medication regimen to achieve those goals.
Our goal here is to help educate and empower patients to establish reasonable and achievable goals; then, in follow-on consults, their RxLive pharmacist can acknowledge and reinforce the patient’s accomplishments to further build confidence and reinforce continued improvements. It’s a process, and one that’s proven effective.
Combatting a lack of motivation — Aligned with The Self-Determination Theory of motivation, pharmacists can increase internal motivation by developing autonomy, competence and relatedness. MI aligned with SDT emphasizes the responsibility and value of patient involvement in their healthcare decision-making, building up their internal motivation to improve adherence. Here, our pharmacists assess patients’ readiness to change, evaluate their personal motivations, what drives their individual behaviors, and determine motivational gaps.
Pharmacists can — and should — provide meaningful information and rational support for change that enables the patient to autonomously determine the importance of their medication regimen, aligning their thoughts with the central values presented. Additionally, during MI, pharmacists can increase motivation by building patient confidence and competence via relatedness. Through the teach-back method and repetitive counseling sessions, pharmacists can instill patient confidence and competence in administration techniques or other teachable components of their regimen.
Further, the level of relatedness patients experience with their healthcare provider affects the likelihood of adhering to recommendations by facilitating an internal behavior change. We impart respect and empathy to gain the trust in patients who may be in a situation outside of their familiarity or comfort zone. Pharmacists are recognized as some as some of the most trusted in the healthcare chain, having a strong opportunity to help patients build autonomy and competence through relatedness and MI to increase their intrinsic motivation for better medication adherence.
Negative beliefs about the plan, healthcare system or diagnosis — We encourage patients to identify and transform their negative beliefs through empathetic listening and MI. We provide knowledge-based professional reasoning on how the medications work to thwart disease progression, discuss self-monitoring techniques or alternatives, and dispel fears about addiction, side effects, or lack of faith in mediations.
Our consulting pharmacists help patients recall and focus on their past positive experiences within the healthcare system, and point to research, innovations, patient choice and empowerment, rapid access, and positive statistics to build confidence and trust. Referrals to support groups and other resources can reinforce all of this information.
Building on life goals — Through patient counseling using MI, pharmacists can explore and emphasize patients’ long-term goals that can be realized through medication adherence and improved lifestyles. We work with patients to create achievable courses of action to improve diet, increase exercise, cease smoking or substance abuse, eliminate triggers, and reduce stress. By reflectively listening, we guide patients to generate their own solutions.
Motivation for what’s not fun — Motivation (or, rather, the lack thereof) impacts behaviors related to health-related activities that most people don’t consider enjoyable, such as regular exercise or better nutrition. (Let’s face it…too many of us would rather eat a pizza or burger than a salad most of the time.) Lack of motivation can surface from multiple sources such as a symptom of an illness, feeling overwhelmed, activity level, difficulty coping, or unmet psychological needs. The Self-Determination Theory suggests that three basic psychological are needed for motivation: autonomy, competence and relatedness. As with the lifestyle choices mentioned below, pharmacists again must help patients put the ‘non-fun stuff” within the broader perspective of living a happier, healthier and longer life.
Lifestyle choices such as smoking and substance abuse (bad!) or maintaining a healthy diet and exercise regimen (good!!) definitely can affect adherence, the number of medications required, and a patient’s adherence to their medication regimen. But we know that some lifestyle behaviors can be addictive and not easily overcome.
And this doesn’t just include the usual “suspects” — smoking, drugs and/or alcohol. Patients must remember that the same is true of foods we know aren’t good for us except in moderation…those containing too many fats, sugars or other carbs. (Remember the potato chip commercial that said “No one can eat just one”? It’s pretty much true, isn’t it?) Not only can foods have a negative impact on our body mass index (BMI) and blood sugar; they can also interact with medications (Biotech), causing adverse effects or interference with absorption.
A resource for support — A pharmacist is also a valuable resource to provide recommendations for appropriate online or local support groups, other healthcare professionals, or cognitive behavioral therapy (CBT) that can assist in recovery or improvement in certain health-related lifestyle areas. In cases of addictive lifestyle behaviors, the pharmacist should notify the provider and cooperatively create strategies to help the patient overcome their barriers and promote adherence.
Summary
A person’s internal social and behavioral factors can have a profound effect on medication adherence and can vary significantly between patients. Pharmacist-directed motivational interviewing during a regular series of consults is an effective way to determine and counter negative beliefs affecting adherence, and to develop and maintain a patient’s positive health-related behaviors.
Resources
Motivational Interviewing for Medication Adherence. American Pharmacists Association
Pharmacies: Improving Health, Reducing Costs. National Association of Chain Drug Stores




